Perimenopause defines a hormone transition period in a woman’s 40s, before she reaches menopause. While this seems like a simple concept, many women in their early 40’s are surprised to discover that the subtle changes in their hormones, metabolism and mood are actually signs of perimenopause. In this article, I want to spell out what exactly happens in perimenopause, when, and what to expect.
I’ll start with a story, from a patient of mine named Christine* (name changed). Christine is in her early 40’s and walks into my office:
“Dr. Kat, I just don’t feel like myself; something feels ‘off’ and I think it might be my hormones. I’m so incredibly irritable during the week before my period, which is so not like me. I feel bad for my kids and my partner because I can’t seem to get a handle on it. I also can’t seem to shake this feeling of anxiety, which is not typical for me. My period has become ridiculously heavy, and I NEVER had that before. I’m waking up every night around 2-3am and can’t get back to sleep. I wake up the next morning feeling completely exhausted. To top it off, I’ve gained about 10lbs, even though I haven’t changed a thing with my diet, and I’m exercising more than ever. My friends are all around age 41-45 like me, and they are feeling similarly… I just don’t feel like MYSELF anymore… what is going on?”
Does this sound familiar?
I can’t tell you the number of times I have heard stories like this from women in my office. Women who are used to feeling familiar and confident in their skin suddenly feel like *something* has shifted but they can’t understand why.
This is a very, very common story for women navigating perimenopause.
In order to understand this hormone transition period, we need to begin by clearing up the confusion with the definition of perimenopause.
Menopause and Perimenopause, Defined
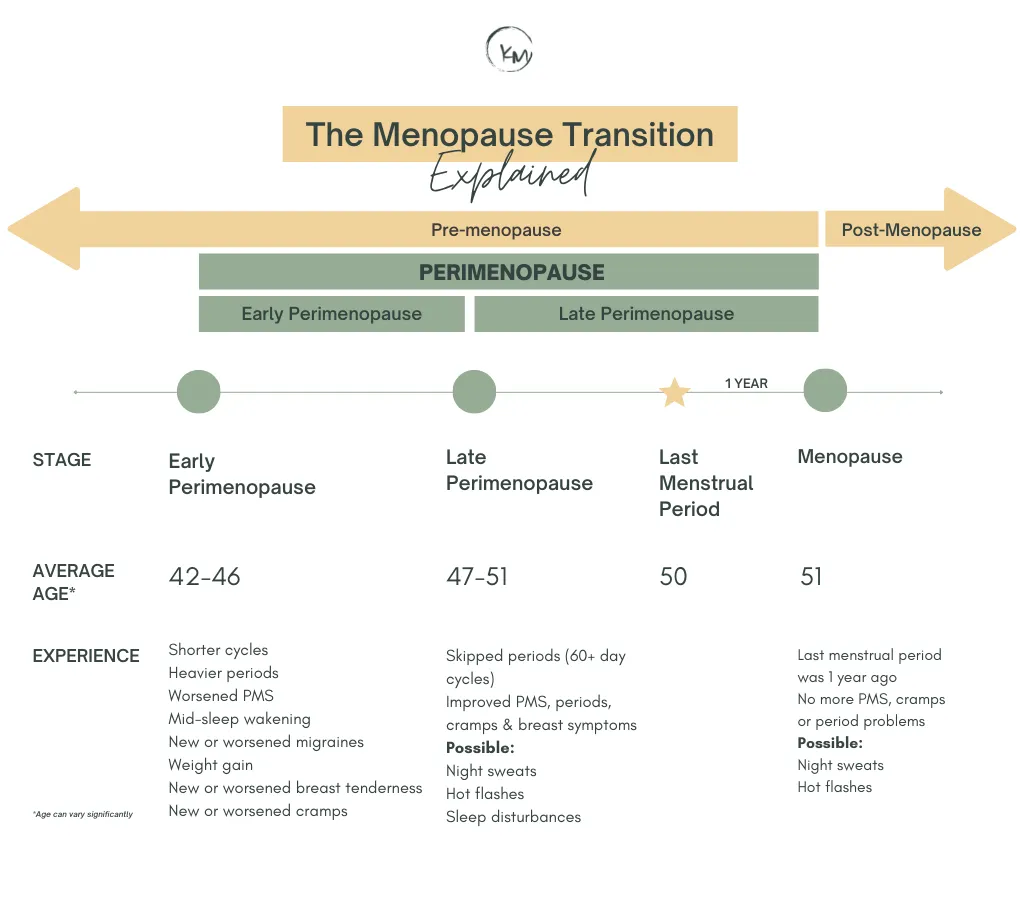
Menopause is defined as a particular point in a woman’s lifetime: she reaches menopause 12 months after her last menstrual period. The average age of menopause is age 51.
Perimenopause defines the years prior to reaching menopause and can begin anywhere from 4 to 9 years before menopause, on average. This means that women may begin noticing the signs of perimenopause in their early 40’s. Perimenopause is divided into two stages: early and late perimenopause. About 80% of women experience hot flashes during this transition, and 20% of women describe this period as “highly symptomatic.” But perimenopause is much more than just hot flashes. Stick with me in this article to understand why.
A few more definitions for you:
Post-menopause defines the remaining decades of a woman’s life after a woman reaches menopause.
You may also hear the term “pre-menopause” used. Pre-menopause is the time of life between puberty, through the reproductive years, until menopause. This definition doesn’t account for perimenopause, which causes some confusion.
I am on a mission to empower women in their 40’s and even late 30’s in understanding how changes in their hormones at this life stage affect not only their menstrual cycle, but also their emotional wellbeing, sleep, metabolism and overall health. This is not just about “managing hot flashes,” this is about developing your body knowledge, recognizing shifts in your hormones early, and getting the right support ASAP so you can continue to feel your best while you navigate this life stage.
Next, I’ll explain the signs and stages of perimenopause, and outline when to seek additional healthcare support.
The Stages of Perimenopause
The perimenopause transition is divided into two stages: early and late perimenopause.
1. Early Perimenopause
Early perimenopause can begin anywhere from approximately 4 to 9 years before menopause (typically around age 42-48). In my experience, I typically see women enter this stage in between age 42 to 45.
During the early perimenopause transition, hormone changes are beginning to occur even though the menstrual cycle doesn’t change at all. Women will still have periods coming at regular intervals in the early stage.
A woman is likely in early perimenopause if she is experiencing any 3 of the following:
- New onset heavy/longer flow
- Shorter menstrual cycles (<26 days)
- New sore, swollen or lumpy breasts
- New mid-sleep wakening
- Increased cramps
- Onset of night sweats, in particular premenstrually (i.e. during the PMS time)
- New or markedly increased migraine headaches
- New or increased premenstrual mood swings
- Weight gain without changes in exercise or eating
As you can see, a 42-year-old woman may be experiencing heavier periods than normal, more irritability at her PMS time, and have worse headaches, not realizing that she is has begun the early stages of perimenopause. What most women don’t know is that perimenopause can begin very subtly. Further, THIS is the ideal time create a health strategy that will help her navigate this transition with ease, rather than waiting and suffering for years before asking for help.
At some point in the early perimenopause stage, the menstrual cycle will eventually become less regular and predictable. An irregular cycle at this stage is defined as a cycle change of 7+ days; for example, your period arriving 7+ days earlier or 7+ days later than it typically does. For example, some women may find that they have months of 24-day cycles, when they typically had a 30-day cycle for most of their life. Or, they may start having a period that arrives 7+ days later than typical for them.
What exactly is happening in early perimenopause?
For most of a woman’s life, the ovaries and the brain are in constant communication. The brain will release a hormone called Follicle Stimulating Hormone (FSH), which “tells” the ovaries to begin preparing a follicle (egg), for ovulation. The egg is released at ovulation, the brain senses this has occurred "as instructed,” and FSH levels stays at relatively low level.
As women progress through their reproductive years, fewer follicles remain to recruit each month. Now, the brain must “yell a little louder” (meaning, release more and more FSH) at the ovaries in order to prepare a follicle for ovulation. We can sometimes see this on a blood test, with elevated FSH levels (more on this later).
With fewer ovulatory cycles, less progesterone is produced. Progesterone is a hormone that helps to normalize the period flow, calm the mood, support sleep and minimize moody PMS symptoms. Therefore, lower progesterone contributes to the experience of moodiness, anxiety, worsened PMS mood swings, disturbed sleep, changes in flow or changes in cycle length (as outlined in the list above). Read here for more information about the “low progesterone” pattern.
At the same time, estrogen levels appear to increase. This is due to the disruption of the typical, cyclic, coordinated timing of messages between the brain and ovaries. This further exacerbates the perimenopause symptoms, particularly lumpy breasts, night sweats or moodiness. The term “estrogen dominance” is sometimes used to describe this pattern of symptoms (click here for more information about estrogen dominance).
How early is “too early” for perimenopause and menopause?
Is it possible to have perimenopause symptoms as early as your 30’s? Yes, it is. When perimenopause symptoms begin this early, we want to pay closer attention. Some women reach menopause early, between the ages of 40-45. This is called Early Menopause.
Less commonly, some women reach menopause very early, before the age of 40. This is called Primary Ovarian Insufficiency (POI). In the cases of both early menopause and POI, the loss of estrogen at this early age can increase the risk of health concerns such as cardiovascular disease, bone loss, and cognitive function concerns. In these cases, it is important to work with a health care provider to address this.
Women with POI or early menopause should discuss with their ND or MD the possible use of Hormone Replacement Therapy (HRT) or Bioidentical Hormone Replacement Therapy (BHRT) to optimize their health and reduce these risks, as a part of their health care plan. I’ll elaborate on this in another article.
2. Late Perimenopause
The late perimenopause transition begins when women begin “skipping” periods or have 2+ months between each period. On average, this may begin around age 47. Women may notice hot flashes or night sweats, in addition to the symptoms described in early perimenopause. Late perimenopause ends after 1 full year without a period; at this point, a woman has reached menopause.
Can you do a blood test for each stage of perimenopause?
As noted above, the hormones FSH can be tested in the blood. However, it is not a reliable marker to depict what stage of perimenopause is occurring. This is because FSH can fluctuate dramatically within a span of a day or more. The same is true of estrogen (estradiol).
One study demonstrated that a random FSH test of >25IU/L is characteristic of late perimenopause; however, FSH is not recommended as a routine test of perimenopause, due to its variability at this time of life.
When women exhibit perimenopause symptoms earlier than expected, for example in their 30’s or early 40’s, additional testing may be recommended to rule out other hormone changes that may mimic perimenopause. This may include a test for thyroid function, prolactin, and a pregnancy screen. Yes, some women report that their perimenopause symptoms actually feel like the early stages of their pregnancies (breast tenderness, moody, weight gain, “missed” periods)!
Since there is no helpful blood test to truly “diagnose” perimenopause, it becomes very important for a woman to be able to recognize the changes in her menstrual cycle, mood, sleep patterns, and overall experience of wellbeing.
This is where working with a Naturopathic Doctor who focusses on hormone health is such an asset. This way, women can have support in understanding WHY they feel the way they do, and more importantly, have a custom health strategy put in place.
This is particularly important for women who are currently on a hormone IUD or taking oral contraceptive pills. These women won’t observe the changes to cycle length or period flow, due to the hormones in their contraception. Therefore, we have to watch out for the other signs of perimenopause, listed above.
By the way, because I am often asked this, and it's a valid question: being on hormonal contraception will not “delay” or “slow” the timing or onset of menopause.
Navigate perimenopause with ease: your unique healthcare plan
I believe that all women should have tailored hormone and health support, but particularly during their 40’s and 50’s. Women at this time of life are up to big things: raising a family, running a business, leaning in at work for leadership positions, or taking on important roles in their community. The last thing you need is to struggle through perimenopause changes without support.
I want you to know that there is a plethora of options to support and manage the perimenopause transition with grace and ease. This includes specific nutrition guidance, herbal medicine, targeted supplements, Bioidentical Hormone Replacement Therapy (BHRT) and many, many other strategies.
To learn more about how you can begin to navigate hormones in your 40’s with ease, check out my free masterclass recording. You’ll also get a copy of the Hormones in your 40’s Mini Guide, with the most important blood tests to have done at this stage.
I have lots more to say about perimenopause, look out for more upcoming articles, coming soon.
Yours in Hormone Health,
Dr Kathleen Mahannah ND
Download your FREE Guide to Hormones in Perimenopause
Learn more about:
The most common hormone imbalances in perimenopause
What stage of perimenopause you're in
The most important TESTS to have done at this stage
Grab your free copy, now!
Dr. Kathleen Mahannah is Naturopathic Doctor licensed by the College of Naturopathic Physicians of British Columbia. Her practice focusses in women's health and hormone balancing using natural medicine and Hormone Therapy, particularly for women in perimenopause and menopause. Dr. Mahannah completed a Degree in Physical Education and Health from University of Toronto, and Diploma of Exercise Science from Capilano College, before obtaining her Diploma of Naturopathic Medicine. She has been practicing for over 6 years in North Vancouver, BC, Canada. Learn more about Dr. Mahannah here.
If you found this article useful, you may enjoy the following articles:
References
Casper, R. (2021) Clinical manifestations and diagnosis of menopause. Retrieved online from UpToDate: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-menopause?search=perimenopause&source=search_result&selectedTitle=1~88&usage_type=default&display_rank=1#H1
Prior JC. Progesterone for Symptomatic Perimenopause Treatment - Progesterone politics, physiology and potential for perimenopause. Facts Views Vis Obgyn. 2011;3(2):109-20. PMID: 24753856; PMCID: PMC3987489.
All content found on this website was created for informational and general educational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your primary care provider or other qualified health professional with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.